

Ischemic optic neuropathies - These include arteritic (Giant Cell Arteritis) and non-arteritic causes.Optic neuritis - Even very mild optic neuritis with a minimal loss of vision can lead to a very strong RAPD.If a condition is bilaterally symmetrical, there will not be an RAPD. Unilateral optic neuropathies are common causes of an RAPD.

Often an extensive loss of peripheral vision correlates with an RAPD.Ĭonditions leading to a Relative Afferent Pupillary Defect include: Optic nerve disorders: Some conditions will lead to a marked reduction of visual acuity with an RAPD, while others spare the central vision. The visual acuity does not necessarily correlate with an RAPD.Because of the consensual light reaction, only one functioning pupil is needed to determine the presence of an RAPD.The diseased eye's pupil will appear to be of equal size to the other eye due to the consensual light reaction (unless the iris itself is diseased or unreactive). Severe disease in one eye leading to an RAPD will not lead to anisocoria.If each eye has severe but equal disease, there will be no RAPD. An RAPD generally occurs with significant optic nerve or retinal disease and when there is a difference in the disease process between the two eyes.Severe Relative Afferent Pupillary Defect: The affected pupil shows an immediate dilation to a greater size.Ĭlick for Interactive Simulations of the Relative Afferent Pupillary Defect(Will open in a separate window) General Discussion Points about the Relative Afferent Pupillary Defect.Moderate Relative Afferent Pupillary Defect: The affected pupil shows a stable or unchanged level of constriction, followed by dilation to a greater size.Mild Relative Afferent Pupillary Defect: The affected pupil shows a weak initial constriction, followed by dilation to a greater size.Hippus refers to non-rhythmic fluctuations in pupillary size when there is a steady illumination. No Relative Afferent Pupillary Defect: Both pupils constrict equally without evidence of pupillary re-dilation with the "swinging flashlight test", except possibly for "hippus".If both eyes are equally dysfunctional, no "relative" defect would be found. Since light in one pupil causes both pupils to constrict, quickly switching from one eye to the other will give a "relative" indication of the functioning of each eye and optic nerve. This is repeated back and forth, until one of four conclusions is reached (listed below). The light is shined into one eye, and then quickly switched to the other. In this test, a strong, steady light is used. The "swinging flashlight test" is probably the best test for identifying an RAPD. In cases where neither pupil reacts to light, no further testing can be done, except for testing the pupillary response to accommodation (focusing at near). In some cases one pupil may not be reactive due to a variety of conditions. It is best to test the individual reaction of each pupil initially. This allows for some pupillary dilation, while also allowing for the observation of the consensual pupillary response.

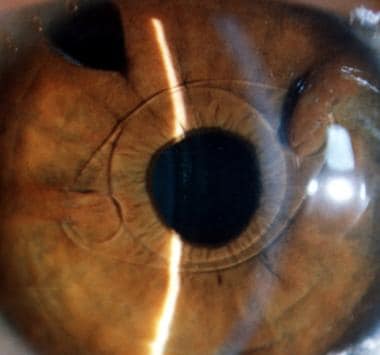
The evaluation of the pupils is best performed in a dimly illuminated room. Finally a list of possible causes of RAPD's as well as conditions that will not cause an RAPD are presented. This page will describe the pupillary examination itself, and through interactive graphics, a variety of examples of RAPD's and even a reverse RAPD will be shown. Also significantly, there are many conditions which lead to a profound loss of vision (such as a complete vitreous hemorrhage), which will not give an RAPD. There are many different conditions which lead to this finding, from severe glaucoma to an optic nerve tumor. Even in an unconscious patient, the determination of an RAPD can be made. The Relative Afferent Pupillary Defect (RAPD), or Marcus-Gunn Pupil is an extremely significant and highly objective clinical finding in the examination of the visual system. Clinical Examination: The Relative Afferent Pupillary Defect
This page is for clinical technical personnel and students and discusses the Relative Afferent Pupillary Defect with interactive demonstrations. Clinical Content: The Relative Afferent Pupillary Defect


 0 kommentar(er)
0 kommentar(er)
